Seasonal Influenza: What You Need to Know
This year the U.S. is experiencing one of the most intense flu seasons in at least 15 years. Public health expert Syra Madad, DH Sc. offers advice on how to protect yourself.
Published February 11, 2025
By Syra Madad, D.H.Sc., M.Sc., MCP, CHEP
Public Health Editor-at-Large

Influenza, or the flu, is a persistent and evolving viral threat that affects millions of Americans annually. This year, the U.S. is experiencing one of the most intense flu seasons in at least 15 years, with flu-related doctor’s visits exceeding the peaks of previous years. According to the Centers for Disease Control and Prevention (CDC), at least 24 million people have been infected so far this season, leading to 310,000 hospitalizations and 13,000 deaths, including 57 pediatric fatalities.
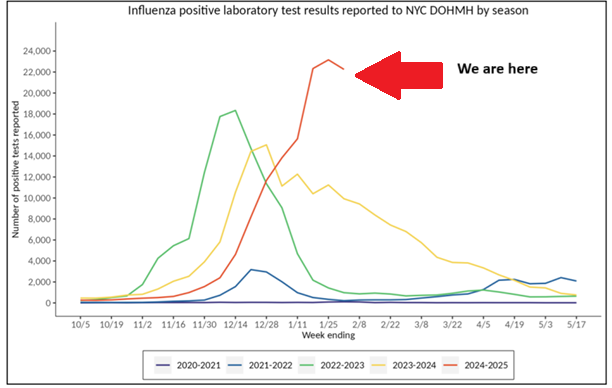
Several states have reported school closures due to high absenteeism among students and staff. While the flu remains most widespread in the South, Southwest, and Western states, significant activity has been reported across 43 states. In New York City, flu activity has reached its peak for this wave, meaning a substantial number of people in the community are experiencing influenza and flu-like symptoms. It will take several weeks for activity to decline locally. On a national level, seasonal flu activity remains elevated and continues to rise in some regions. However, it’s not too late to get vaccinated. With flu transmission still high, getting vaccinated can provide meaningful protection for both individuals and communities.
How the Flu Spreads and What to Expect
Influenza is highly contagious and spreads easily through close contact with an infected person. The virus is primarily transmitted through droplets released when a sick person coughs, sneezes, or talks. Infection occurs when these droplets, or contaminated saliva or mucus, enter the eyes, nose, or mouth. It can also spread by touching virus-contaminated surfaces and then touching the face. Given its rapid transmission, understanding flu symptoms, prevention strategies, and available treatments are key to minimizing its impact. Here’s what you need to know:
Key Information
| Incubation Period | 1–4 days after exposure before symptoms appear. |
| Contagious Period | 1 day before symptoms to up to 7 days after onset; longer in children and immunocompromised individuals. Most contagious in the first 3 days |
| Signs & Symptoms | Fever, chills, cough, sore throat, body aches, fatigue, headache, congestion; vomiting/diarrhea more common in children. |
| Isolation Period | Stay home until symptoms improve and fever-free for 24 hours without medication. |
| Prevention | Annual flu vaccine, handwashing, avoiding sick individuals, mask-wearing in crowds, improving ventilation, and disinfecting surfaces. |
| Treatment | Rest, hydration, antivirals (e.g., oseltamivir) for high-risk or severe cases, most effective within 48 hours of symptoms. |
| Flu Vaccine Eligibility | Everyone aged six months and older |
| High-Risk Groups | Young children, older adults, pregnant individuals, and those with chronic conditions or weakened immunity. |
| Where to Get Vaccinated (NYC) | NYC Vaccine Finder, pharmacies, doctor’s offices, clinics, employer programs. Find a flu vaccine at vaccinefinder.nyc.gov |
| Where to Get Vaccinated (Outside NYC) | Pharmacies (CVS, Walgreens, Rite Aid), primary care offices, urgent care centers, health departments. Find a flu vaccine at vaccines.gov |
| Who Should Get Vaccinated | Everyone 6 months+, especially high-risk groups; high-dose options available for older adults. |
| When to Seek Medical Attention for Emergency Symptoms | Breathing issues, chest pain, dehydration, confusion, worsening symptoms, or fever >3 days or stays above 104°F. In children, rapid breathing, flaring nostrils, difficulty drinking fluids, dehydration, any fever in infants under 3 months, unusual fussiness or poor feeding |
Why the Flu Vaccine Matters
Vaccination is the best defense against severe illness, hospitalization, and complications from influenza, particularly for those with chronic health conditions. In recent flu seasons, 9 out of 10 people hospitalized with flu had at least one underlying condition, highlighting the importance of annual vaccination for high-risk individuals.
While flu vaccine effectiveness varies each year, research shows that during seasons when vaccine strains closely match circulating viruses, vaccination reduces the risk of flu illness by 40–60% and related hospitalization by 60%. Even in years with a suboptimal match, vaccination helps reduce symptom severity, prevents associated complications like pneumonia, and lowers the risk of worsening chronic conditions.
Flu vaccines have also been shown to significantly reduce the severity of illness. A 2018 study found that from 2012 to 2015, flu vaccination among adults reduced the risk of being admitted to an intensive care unit (ICU) with flu by 82%. Similarly, a 2014 study showed that flu vaccination reduced children’s risk of flu-related pediatric intensive care unit (PICU) admission by 74% during the 2010–2012 flu seasons.
Flu vaccines protect against three different influenza viruses (two influenza A strains and one influenza B strain), and since multiple influenza viruses often circulate in a single season, vaccination remains essential. Ongoing studies continue to show that even when vaccinated individuals contract the flu, their illness tends to be less severe.
The Bottom Line: Protect Yourself and Others
Influenza poses a serious risk, especially to vulnerable populations. With over 13,000 flu-related deaths recorded this season and numbers expected to rise, taking preventive measures is critical. If you haven’t gotten your flu shot yet, it’s not too late, flu activity remains high, and vaccination can still provide protection.
Stay connected with Dr. Madad:
Instagram
Twitter/X
LinkedIn
Facebook
